Understanding Glaucoma: Decoding the Intraocular Strain (IOP) Chart
Associated Articles: Understanding Glaucoma: Decoding the Intraocular Strain (IOP) Chart
Introduction
With enthusiasm, let’s navigate via the intriguing matter associated to Understanding Glaucoma: Decoding the Intraocular Strain (IOP) Chart. Let’s weave attention-grabbing info and supply contemporary views to the readers.
Desk of Content material
Understanding Glaucoma: Decoding the Intraocular Strain (IOP) Chart
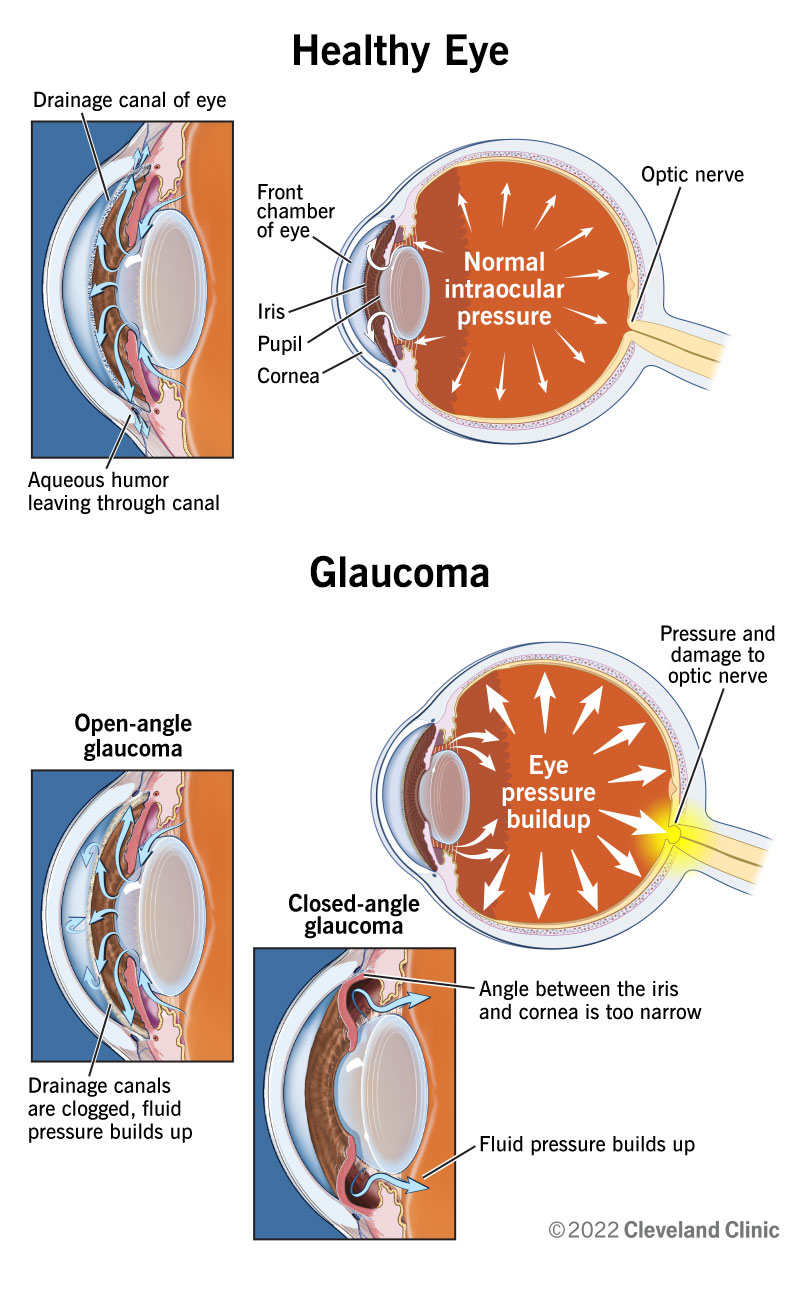
Glaucoma, a number one explanation for irreversible blindness worldwide, is characterised by harm to the optic nerve, usually related to elevated intraocular strain (IOP). Whereas IOP is an important think about glaucoma, it is not the one one; a posh interaction of genetic predisposition, age, and different elements contributes to its growth. Understanding the connection between IOP and glaucoma danger requires a nuanced strategy, going past merely taking a look at a strain vary chart. This text delves into the complexities of IOP measurement, its interpretation within the context of glaucoma, and the constraints of relying solely on IOP as a diagnostic instrument.
What’s Intraocular Strain (IOP)?
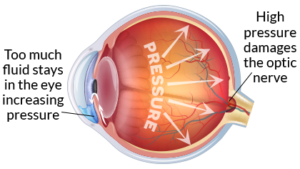
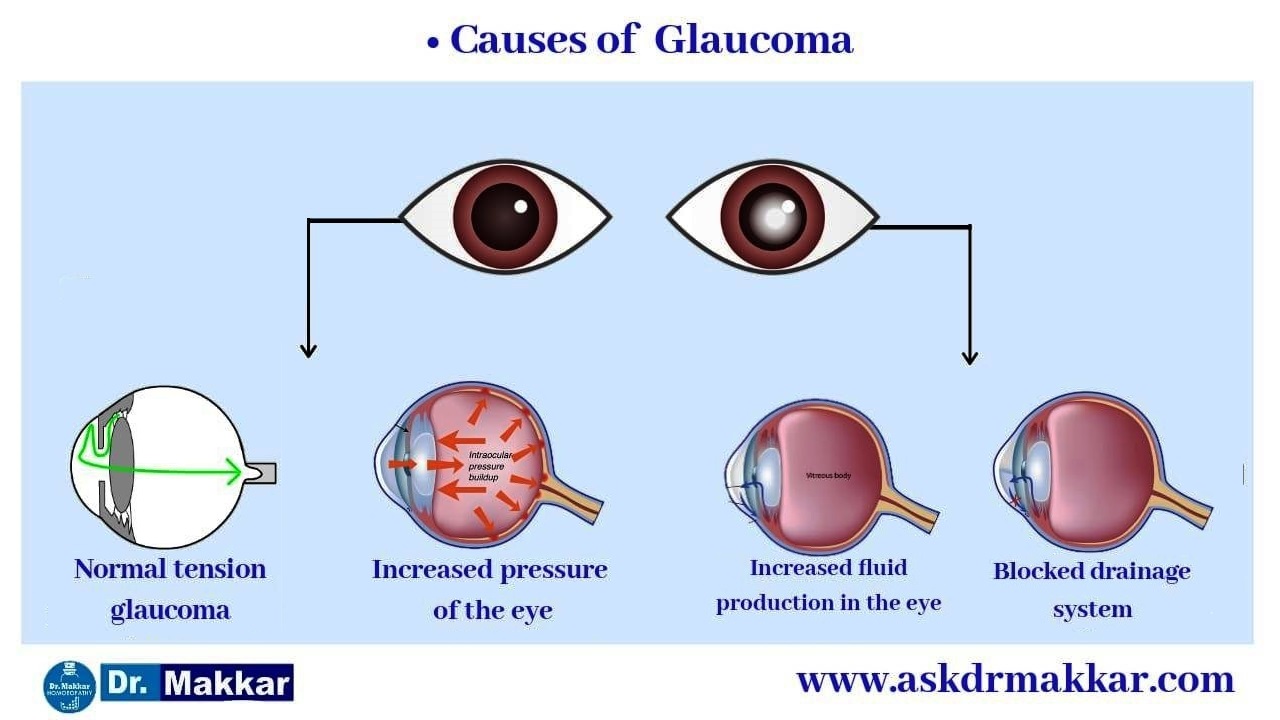
IOP refers back to the fluid strain inside the attention. This strain is maintained by a fragile steadiness between the manufacturing and outflow of aqueous humor, a transparent fluid that nourishes the attention’s tissues. The aqueous humor is produced by the ciliary physique and flows via the pupil into the anterior chamber (the house between the iris and cornea). It then drains out via a community of channels known as the trabecular meshwork and Schlemm’s canal. Any disruption on this delicate steadiness can result in elevated IOP.
Measuring Intraocular Strain (IOP): Tonometry Strategies
Correct IOP measurement is essential for glaucoma analysis and administration. A number of strategies are used, every with its personal benefits and limitations:
-
Applanation Tonometry (Goldmann Applanation Tonometry): That is the gold commonplace, thought of essentially the most correct methodology. It entails flattening a small space of the cornea utilizing a standardized pressure, and the strain required to attain this flattening is measured. It requires specialised tools and experience.
-
Non-contact Tonometry (NCT): This methodology makes use of a puff of air to indent the cornea, measuring the strain primarily based on the rebound. It is quicker and fewer invasive than applanation tonometry however could be much less correct, notably in eyes with corneal irregularities.
-
Rebound Tonometry (Icare Tonometer): This moveable gadget makes use of a small probe to softly indent the cornea and measures the rebound pressure. It is handy for bedside use and fewer invasive than applanation tonometry however can nonetheless be affected by corneal thickness and stiffness.
-
Tonopen: This gadget makes use of a small probe to measure IOP. It’s thought of extra correct than NCT however much less correct than Goldmann applanation tonometry.
The selection of tonometry methodology is dependent upon elements like affected person consolation, availability of apparatus, and the clinician’s experience. Whatever the methodology used, correct measurements require a talented technician and cautious consideration to element.
The IOP Vary Chart: A Simplified View
Whereas there is not a universally accepted "regular" IOP vary, it is usually thought of to be between 10 and 21 mmHg (millimeters of mercury). Nevertheless, this can be a very simplified illustration and shouldn’t be interpreted in isolation. Many people with IOP inside this vary can develop glaucoma, whereas others with IOP barely above this vary might not. The "IOP vary chart" is subsequently a deceptive simplification.
The Limitations of Relying Solely on IOP:
IOP is only one piece of the puzzle in glaucoma analysis and administration. A number of limitations exist in relying solely on IOP measurements:
-
Regular Stress Glaucoma (NTG): Such a glaucoma happens in people with IOP inside the "regular" vary (usually under 21 mmHg). The precise trigger is unknown, but it surely means that elements past IOP contribute to optic nerve harm.
-
Ocular Hypertension: This situation refers to elevated IOP with none seen optic nerve harm or visible discipline loss. Not everybody with ocular hypertension will develop glaucoma, but it surely will increase the danger. Common monitoring is essential to detect early indicators of glaucoma.
-
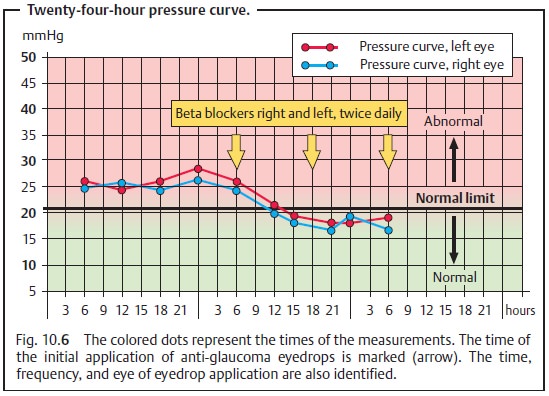
Variability of IOP: IOP fluctuates all through the day, influenced by elements corresponding to posture, time of day, and medicine. A single IOP measurement might not precisely replicate the common IOP. A number of measurements over time are important for a dependable evaluation.
-
Corneal Thickness: Corneal thickness impacts IOP measurements. Thicker corneas can result in falsely elevated IOP readings, whereas thinner corneas can result in falsely low readings. Fashionable tonometers usually appropriate for corneal thickness, however this correction shouldn’t be all the time excellent.
-
Different Elements: Genetic predisposition, age, race, and different underlying well being situations can affect glaucoma danger, impartial of IOP.
Past IOP: Different Diagnostic Instruments for Glaucoma
A complete glaucoma analysis goes past IOP measurement. It entails:
-
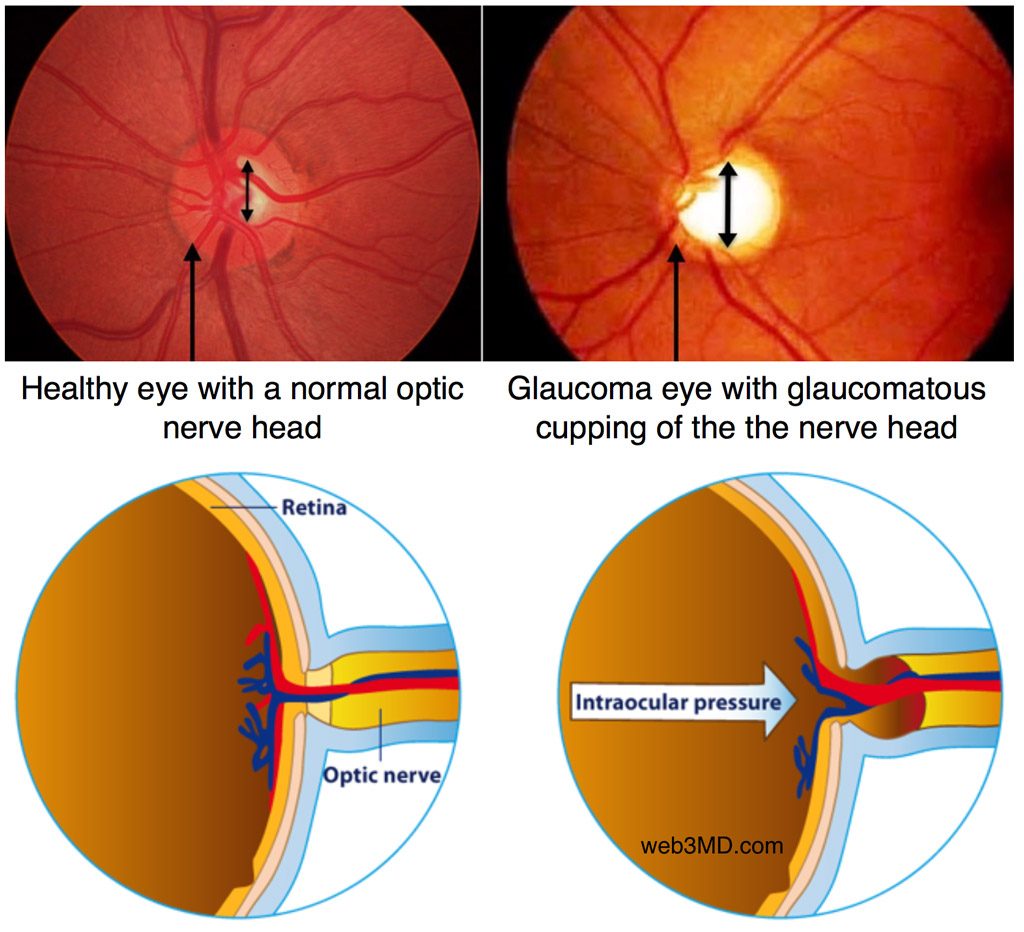
Optic Nerve Examination: Detailed examination of the optic nerve head utilizing ophthalmoscopy and optical coherence tomography (OCT) helps assess the presence and extent of optic nerve harm. OCT gives high-resolution pictures of the optic nerve, permitting for exact measurement of retinal nerve fiber layer (RNFL) thickness.
-
Visible Area Testing (Perimetry): This take a look at assesses the extent of peripheral imaginative and prescient. Glaucoma usually causes progressive lack of peripheral imaginative and prescient, which could be detected via perimetry. Various kinds of perimetry exist, every with its personal benefits and limitations.
-
Gonioscopy: This examination makes use of a particular lens to visualise the angle the place the iris meets the cornea. It helps assess the drainage angle of the aqueous humor and establish any structural abnormalities that will contribute to elevated IOP.
Glaucoma Administration: A Personalised Method
Glaucoma administration goals to forestall additional optic nerve harm and protect imaginative and prescient. The remedy strategy is customized primarily based on numerous elements, together with IOP stage, the speed of IOP development, the severity of optic nerve harm, and the affected person’s total well being.
Therapy choices might embrace:
-
Drugs: Eye drops are the first-line remedy for many glaucoma sufferers. These drugs both cut back aqueous humor manufacturing or improve its outflow.
-
Laser Remedy: Laser procedures, corresponding to laser peripheral iridotomy (LPI) and selective laser trabeculoplasty (SLT), can enhance aqueous humor outflow.
-
Surgical procedure: Surgical interventions, corresponding to trabeculectomy or glaucoma drainage implants, could also be mandatory if medical remedy fails to manage IOP adequately.
Conclusion:
Whereas an IOP vary chart gives a simplified overview, it’s essential to grasp its limitations. Glaucoma analysis and administration require a holistic strategy, contemplating numerous elements past IOP, together with optic nerve standing, visible discipline modifications, and particular person affected person traits. Common eye exams are important for early detection and well timed intervention, considerably bettering the possibilities of preserving imaginative and prescient. Relying solely on a numerical IOP worth to evaluate glaucoma danger is inaccurate and probably dangerous. An intensive examination by an ophthalmologist is paramount for correct analysis and efficient administration of this sight-threatening situation. The main focus needs to be on preserving imaginative and prescient, not solely on attaining a selected IOP goal. The connection between IOP and glaucoma is complicated, and a collaborative strategy between the ophthalmologist and the affected person is important for profitable long-term administration.




Closure
Thus, we hope this text has supplied precious insights into Understanding Glaucoma: Decoding the Intraocular Strain (IOP) Chart. We thanks for taking the time to learn this text. See you in our subsequent article!